Program Manager Quality Strategy
The posted compensation range of $34.50 - $49.04 /hour is a reasonable estimate that extends from the lowest to the highest pay 91В鶹№ъІъѕ«Ж·ЧФЕД in good faith believes it might pay for this particular job, based on the circumstances at the time of posting. 91В鶹№ъІъѕ«Ж·ЧФЕД may ultimately pay more or less than the posted range as permitted by law.
The purpose of Dignity Health Management Services Organization (Dignity Health MSO) is to build a system-wide integrated physician-centric full-service management service organization structure. We offer a menu of management and business services that will leverage economies of scale across provider types and geographies and will lead the effort in developing Dignity Health’s Medicaid population health care management pathways. Dignity Health MSO is dedicated to providing quality managed care administrative and clinical services to medical groups hospitals health plans and employers with a business objective to excel in coordinating patient care in a manner that supports containing costs while continually improving quality of care and levels of service. Dignity Health MSO accomplishes this by capitalizing on industry-leading technology and integrated administrative systems powered by local human resources that put patient care first.
Dignity Health MSO offers an outstanding Total Rewards package that integrates competitive pay with a state-of-the-art flexible Health & Welfare benefits package. Our cafeteria-style benefit program gives employees the ability to choose the benefits they want from a variety of options including medical dental and vision plans for the employee and their dependents Health Spending Account (HSA) Life Insurance and Long Term Disability. We also offer a 401k retirement plan with a generous employer-match. Other benefits include Paid Time Off and Sick Leave.
Arizona Care Network (ACN) is a clinically integrated (CI) physician network and Accountable Care Organization (ACO) sponsored by Dignity Health and Abrazo Health.
Responsibilities
***This position is hybrid in-office and work from home.
Position Summary:
Arizona Care Network (ACN) is a clinically integrated (CI) physician network and Accountable Care Organization (ACO) sponsored by Dignity Health and Abrazo Health. The Program Manager, Quality Strategy is an employee of Dignity Health Managed Services Organization (DHMSO), a wholly owned subsidiary of Dignity Health.
The Quality Strategy Program Manager is responsible for leading quality strategy initiatives including, but not limited to, the following:
•Defining and executing quality improvement strategies
•Defining and executing utilization management strategies (ED visits, inpatient utilization, readmissions,etc.)
•Provider-Patient resource program developer
•Developing relationships with practices and facilities to encourage adoption of strategies
•Facilitating provider and facility education on quality and utilization metric
•Social media strategist
•Content Library editor and publisher
•Texting Platforms organization and management
Responsibilities may include:
- In collaboration with the Quality Manager, lead the development and implementation of the organization's quality strategy, aligning it with business goals and objectives. Collaborate with cross-functional teams to establish comprehensive quality improvement plans, identifying key performance indicators (KPIs), metrics, and benchmarks. Texting, social media, and emails are one component of a communication strategy.
- Ensure compliance with industry regulations, standards, and best practices. Establish and maintain quality assurance procedures, conducting regular audits and assessments to ensure adherence to established quality frameworks.
- Develop and implement comprehensive communication strategies aligned with overall quality measures campaigns and business objectives, which may include phone calls, social media, emails, and in person events.
- Create and manage personalized texting campaigns following quality measures and health program initiatives.
- Development and management of engaging, relevant, and high-quality content as well as facilitating education to practices and facilities.
- Develop external/internal PowerPoint presentations and creation of provider/patient resources.
- Plan and execute social media strategies, such as individualized disease management messages, departmental events, tracking engagement, and prompt responses to comments and messages.
- Plan and carry out texting/call initiatives, including personalized disease management and education, appointment oriented messaging, and quality measures to close gaps.
- Analysis and performance tracking for outreach campaigns, social media posts, quality strategies, and identify data trends for improvement opportunities.
- Works collaboratively with ACN’s Director of Analytics and with appropriate data/analytics vendors to design and build metrics and dashboard reports that allow for regular tracking of program performance, and the implementation of improvement opportunities throughout the network.
- Perform other duties as assigned including but not limited to GPRO and HEDIS audits, collects and summarize performance data, outreach members, perform medical record reviews, identify opportunities for improvement, and present findings as needed.
Qualifications
Minimum Qualifications:
- Minimum 2 years’ experience in quality improvement techniques.
- Able to summarize data findings concisely for internal and external stakeholders; able to make inferences and offer suggestions for improvements.
- Bachelor's degree in a relevant field
- Knowledgeable of Accountable Care Organization requirements and structures.
- Must have excellent verbal and written communication skills; a solid knowledge of budgeting and financial practices.
- Must be able to communicate and interface effectively with internal and external customers.
- Proficiency with the Microsoft Office suite of applications.
Preferred Qualifications:
- Master’s in Business Administration or equivalent degree preferred
Unless directed by a Collective Bargaining Agreement, applications for this position will be considered on a rolling basis. 91В鶹№ъІъѕ«Ж·ЧФЕД cannot anticipate the date by which a successful candidate may be identified.
Depending on the position offered, 91В鶹№ъІъѕ«Ж·ЧФЕД offers a generous benefit package, including but not limited to medical, prescription drug, dental, vision plans, life insurance, paid time off (full-time benefit eligible employees may receive a minimum of 14 paid time off days, including holidays annually), tuition reimbursement, retirement plan benefit(s) including, but not limited to, 401(k), 403(b), and other defined benefits offerings, as may be amended from time to time. For more information, please visit /benefits.
No featured jobs
No recently viewed jobs
You have no saved jobs
-

-
 Our Mission and Vision 91В鶹№ъІъѕ«Ж·ЧФЕД was created by the alignment of health care organizations to serve as a single ministry of change.
Our Mission and Vision 91В鶹№ъІъѕ«Ж·ЧФЕД was created by the alignment of health care organizations to serve as a single ministry of change. -
 Diversity & Inclusion At 91В鶹№ъІъѕ«Ж·ЧФЕД, we are dedicated to delivering humankindness. Diversity is not just an initiative, it’s the true nature of who we are. Related Content
Diversity & Inclusion At 91В鶹№ъІъѕ«Ж·ЧФЕД, we are dedicated to delivering humankindness. Diversity is not just an initiative, it’s the true nature of who we are. Related Content -

-

-

-
 Nursing Explore more about nursing opportunities, our nursing vision and hear from our staff members. Related Content
Nursing Explore more about nursing opportunities, our nursing vision and hear from our staff members. Related Content -
 Our Benefits Our benefits and perks are a big part of why we’re ranked a top employer. Related Content
Our Benefits Our benefits and perks are a big part of why we’re ranked a top employer. Related Content -

-

-

-

-

-

-
 Saved Jobs Saved Jobs
Saved Jobs Saved Jobs -
 Legal and Privacy Notices Legal and Privacy Notices
Legal and Privacy Notices Legal and Privacy Notices -
 Terms of Service Terms of Service
Terms of Service Terms of Service -
 Website Privacy Notice Website Privacy Notice
Website Privacy Notice Website Privacy Notice -
 Online Accessibility Notice Online Accessibility Notice
Online Accessibility Notice Online Accessibility Notice -
 Copyrights Copyrights
Copyrights Copyrights -
 Application Notices and Information Application Notices and Information
Application Notices and Information Application Notices and Information -
 National Nursing New Grad Residency Program Learn about our new grad nursing program that is nationally-standardized and evidence-based best practice for newly licensed nurses Hiring Process
National Nursing New Grad Residency Program Learn about our new grad nursing program that is nationally-standardized and evidence-based best practice for newly licensed nurses Hiring Process -
 91В鶹№ъІъѕ«Ж·ЧФЕД Alumni Community Interested in returning to 91В鶹№ъІъѕ«Ж·ЧФЕД? Learn about jobs, company news, and hear from our employees. Hiring Process
91В鶹№ъІъѕ«Ж·ЧФЕД Alumni Community Interested in returning to 91В鶹№ъІъѕ«Ж·ЧФЕД? Learn about jobs, company news, and hear from our employees. Hiring Process -
 Mission Administrative Fellowship at 91В鶹№ъІъѕ«Ж·ЧФЕД Explore your career path and learn about our Mission Administrative Fellowship Hiring Process
Mission Administrative Fellowship at 91В鶹№ъІъѕ«Ж·ЧФЕД Explore your career path and learn about our Mission Administrative Fellowship Hiring Process -
 Your career in Environmental Services at 91В鶹№ъІъѕ«Ж·ЧФЕД Explore a career in EVS and learn how to grow your career in healthcare. Hiring Process
Your career in Environmental Services at 91В鶹№ъІъѕ«Ж·ЧФЕД Explore a career in EVS and learn how to grow your career in healthcare. Hiring Process -
 Operations Track .The 91В鶹№ъІъѕ«Ж·ЧФЕД Administrative Fellowship Operations Track will provide fellows with a broad range of health care experiences at the national and local level.
Operations Track .The 91В鶹№ъІъѕ«Ж·ЧФЕД Administrative Fellowship Operations Track will provide fellows with a broad range of health care experiences at the national and local level. -
 Information Technology The 91В鶹№ъІъѕ«Ж·ЧФЕД Administrative Fellowship Information Technology (IT) Track will provide fellows with a broad range of experiences in information technology within an integrated health care system.
Information Technology The 91В鶹№ъІъѕ«Ж·ЧФЕД Administrative Fellowship Information Technology (IT) Track will provide fellows with a broad range of experiences in information technology within an integrated health care system. -
 Mission Track The 91В鶹№ъІъѕ«Ж·ЧФЕД Administrative Fellowship Mission Track Fellow will work directly with mission leadership to develop leadership competencies in Mission Integration, Spiritual Care, Community Health, Ethics, and Ministry Formation.
Mission Track The 91В鶹№ъІъѕ«Ж·ЧФЕД Administrative Fellowship Mission Track Fellow will work directly with mission leadership to develop leadership competencies in Mission Integration, Spiritual Care, Community Health, Ethics, and Ministry Formation. -

-
 Military At 91В鶹№ъІъѕ«Ж·ЧФЕД, we deeply value the sacrifices made by our veterans and their families. Our commitment to supporting those who served extends beyond words—reflected in the opportunities and benefits we provide. Related Content
Military At 91В鶹№ъІъѕ«Ж·ЧФЕД, we deeply value the sacrifices made by our veterans and their families. Our commitment to supporting those who served extends beyond words—reflected in the opportunities and benefits we provide. Related Content -
 VMFH Hiring our Heroes VMFH HIring our Heroes
VMFH Hiring our Heroes VMFH HIring our Heroes -
 Meet the Fellows Meet our current 91В鶹№ъІъѕ«Ж·ЧФЕД Fellows. This is a national, 18-month, system-wide leadership and professional development program that offers a solid foundation for future leaders through hands-on learning experiences, exposure to clinical and non-clinical aspects and mentoring from influential innovators. News/Advancements
Meet the Fellows Meet our current 91В鶹№ъІъѕ«Ж·ЧФЕД Fellows. This is a national, 18-month, system-wide leadership and professional development program that offers a solid foundation for future leaders through hands-on learning experiences, exposure to clinical and non-clinical aspects and mentoring from influential innovators. News/Advancements -
 On Demand Staffing On Demand Staffing at 91В鶹№ъІъѕ«Ж·ЧФЕД offers flexible schedules for nurses News/Advancements
On Demand Staffing On Demand Staffing at 91В鶹№ъІъѕ«Ж·ЧФЕД offers flexible schedules for nurses News/Advancements -
 COVID-19 Vaccination Requirements COVID-19 Vaccination Requirements at 91В鶹№ъІъѕ«Ж·ЧФЕД
COVID-19 Vaccination Requirements COVID-19 Vaccination Requirements at 91В鶹№ъІъѕ«Ж·ЧФЕД -
 Your career in Clinical Engineering at 91В鶹№ъІъѕ«Ж·ЧФЕД A career in clinical engineering offers a fulfilling blend of technology and healthcare, with the potential to make a positive impact on patient outcomes and the overall efficiency of healthcare delivery. Learn more and explore a career in clinical engineering at 91В鶹№ъІъѕ«Ж·ЧФЕД. Hiring Process
Your career in Clinical Engineering at 91В鶹№ъІъѕ«Ж·ЧФЕД A career in clinical engineering offers a fulfilling blend of technology and healthcare, with the potential to make a positive impact on patient outcomes and the overall efficiency of healthcare delivery. Learn more and explore a career in clinical engineering at 91В鶹№ъІъѕ«Ж·ЧФЕД. Hiring Process -
 CSH Acts of Humankindness Acts of Humankindness. These are the Acts of Humankindness that bring our mission to life. Hiring Process
CSH Acts of Humankindness Acts of Humankindness. These are the Acts of Humankindness that bring our mission to life. Hiring Process -
 91В鶹№ъІъѕ«Ж·ЧФЕД hiring our heroes 12-week Hiring Our Heroes Corporate Fellowship Program. Our first 91В鶹№ъІъѕ«Ж·ЧФЕД’s first graduate. Hiring Process
91В鶹№ъІъѕ«Ж·ЧФЕД hiring our heroes 12-week Hiring Our Heroes Corporate Fellowship Program. Our first 91В鶹№ъІъѕ«Ж·ЧФЕД’s first graduate. Hiring Process -
 CHI Health 2025 Nursing Internship CHI Health Nursing Internship in Nebraska Hiring Process
CHI Health 2025 Nursing Internship CHI Health Nursing Internship in Nebraska Hiring Process -
 Upper Midwest Now is the perfect time to join our healthcare team in one of our Upper Midwest locations in Minnesota and North Dakota! Hiring Process
Upper Midwest Now is the perfect time to join our healthcare team in one of our Upper Midwest locations in Minnesota and North Dakota! Hiring Process -
 CHI Health Career Ladder CNA Program CHI Health has partnered with local Certified Nursing Assistant Programs to offer students C.N.A. training in exchange for full or part-time employment! Hiring Process
CHI Health Career Ladder CNA Program CHI Health has partnered with local Certified Nursing Assistant Programs to offer students C.N.A. training in exchange for full or part-time employment! Hiring Process -
 CHI Acts of Humankindness Acts of Humankindness. These are the Acts of Humankindness that bring our mission to life. Hiring Process
CHI Acts of Humankindness Acts of Humankindness. These are the Acts of Humankindness that bring our mission to life. Hiring Process -
 Dignity Health California Workplace Diversity Award Dignity Health (California) has been recognized as one of America’s Greatest Workplaces for Diversity 2023 by Newsweek and Plant-A Insights Group. Diversity
Dignity Health California Workplace Diversity Award Dignity Health (California) has been recognized as one of America’s Greatest Workplaces for Diversity 2023 by Newsweek and Plant-A Insights Group. Diversity -
 New Grad Nurse Residency and Transition Program for RNs in California Learn about New Grad Residency and Transition or Fellowship Program for RNs in California Hiring Process
New Grad Nurse Residency and Transition Program for RNs in California Learn about New Grad Residency and Transition or Fellowship Program for RNs in California Hiring Process -
 DHMF benefits at a glance 2024 non represented DHMF benefits at a glance 2024 (non-represented)
DHMF benefits at a glance 2024 non represented DHMF benefits at a glance 2024 (non-represented) -
 DH Acts of Humankindness Acts of Humankindness. These are the Acts of Humankindness that bring our mission to life. Hiring Process
DH Acts of Humankindness Acts of Humankindness. These are the Acts of Humankindness that bring our mission to life. Hiring Process -
 DHMSO benefits at a glance 2024 DHMSO benefits at a glance 2024
DHMSO benefits at a glance 2024 DHMSO benefits at a glance 2024 -
 DHMF CNA Represented benefits 2024 DHMF CNA Represented benefits 2024
DHMF CNA Represented benefits 2024 DHMF CNA Represented benefits 2024 -
 DHMF Woodland Benefits 2024 Non Represented DHMF Woodland Benefits 2024 Non Represented
DHMF Woodland Benefits 2024 Non Represented DHMF Woodland Benefits 2024 Non Represented -
 DHMF Benefits Summary 2024 SEIU Represented DHMF Benefits Summary 2024 SEIU Represented
DHMF Benefits Summary 2024 SEIU Represented DHMF Benefits Summary 2024 SEIU Represented -
 91В鶹№ъІъѕ«Ж·ЧФЕД is Advancing Equitable Opportunities for Hiring and Training 91В鶹№ъІъѕ«Ж·ЧФЕД is engaged in the Healthcare Anchor Network’s Impact Workforce Commitment, an initiative to hire and train individuals who may have faced employment barriers due to low income, lack of access to education and training, and other socioeconomic challenges. Hiring Process
91В鶹№ъІъѕ«Ж·ЧФЕД is Advancing Equitable Opportunities for Hiring and Training 91В鶹№ъІъѕ«Ж·ЧФЕД is engaged in the Healthcare Anchor Network’s Impact Workforce Commitment, an initiative to hire and train individuals who may have faced employment barriers due to low income, lack of access to education and training, and other socioeconomic challenges. Hiring Process -
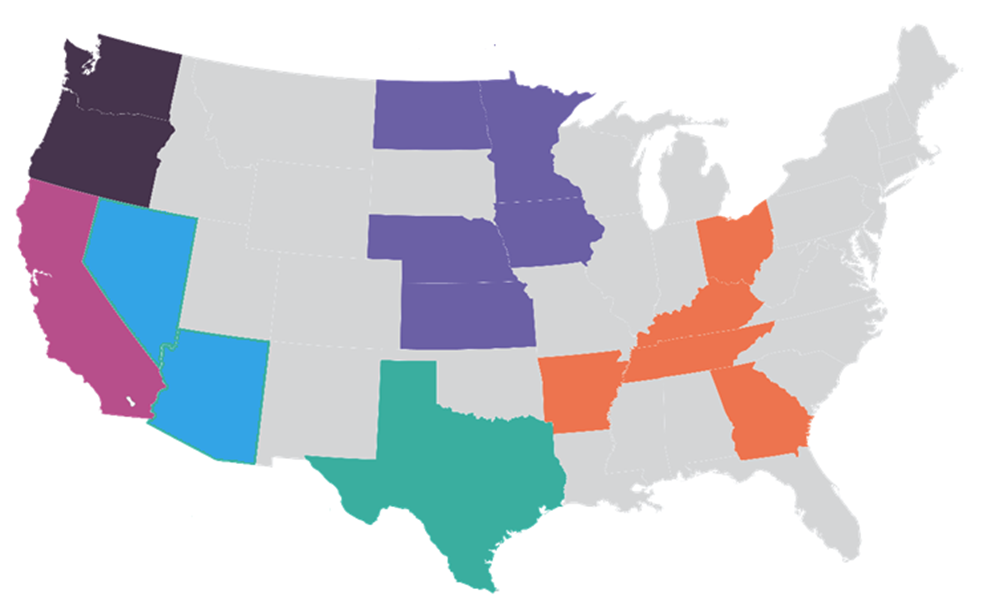
 CHI Health Locations Now is the perfect time to join our CHI team in one of our locations! Hiring Process
CHI Health Locations Now is the perfect time to join our CHI team in one of our locations! Hiring Process -
 Your career as a Medical Assistant at 91В鶹№ъІъѕ«Ж·ЧФЕД Learn about a career as a Medical Assistant and explore how to grow your career at 91В鶹№ъІъѕ«Ж·ЧФЕД Hiring Process
Your career as a Medical Assistant at 91В鶹№ъІъѕ«Ж·ЧФЕД Learn about a career as a Medical Assistant and explore how to grow your career at 91В鶹№ъІъѕ«Ж·ЧФЕД Hiring Process -
 VMFH Acts of Humankindness Acts of Humankindness. These are the Acts of Humankindness that bring our mission to life. Article Hiring Process
VMFH Acts of Humankindness Acts of Humankindness. These are the Acts of Humankindness that bring our mission to life. Article Hiring Process -
 Learn about our National Travel Nurse Program Join our National Travel Nursing Program and enjoy the variety of a travel nurse with the security of being employed by one of the largest faith-based healthcare systems in the country.
Learn about our National Travel Nurse Program Join our National Travel Nursing Program and enjoy the variety of a travel nurse with the security of being employed by one of the largest faith-based healthcare systems in the country. -
 Learn about our Virtually Integrated Nursing Care Model Virtually Integrated Care provides assistance to the bedside team and patient/family through the use of virtual technology
Learn about our Virtually Integrated Nursing Care Model Virtually Integrated Care provides assistance to the bedside team and patient/family through the use of virtual technology -
 91В鶹№ъІъѕ«Ж·ЧФЕД and NAHSE 2024 Join 91В鶹№ъІъѕ«Ж·ЧФЕД at the 38th Annual NAHSE conference, where we are proud partners, for a unique opportunity to connect with fellow professionals and leaders in the healthcare industry.
91В鶹№ъІъѕ«Ж·ЧФЕД and NAHSE 2024 Join 91В鶹№ъІъѕ«Ж·ЧФЕД at the 38th Annual NAHSE conference, where we are proud partners, for a unique opportunity to connect with fellow professionals and leaders in the healthcare industry. -
 SoCal Benefits at a Glance 2024 SoCal Benefits at a Glance 2024
SoCal Benefits at a Glance 2024 SoCal Benefits at a Glance 2024 -
 Innovative Virtual Nursing Model 91В鶹№ъІъѕ«Ж·ЧФЕД has two types of virtual nurses: ones who work at a command center to help with admissions, discharges and transfers, and ones who are part of the care team, attending rounds with physicians and being available to patients at the push of the button.
Innovative Virtual Nursing Model 91В鶹№ъІъѕ«Ж·ЧФЕД has two types of virtual nurses: ones who work at a command center to help with admissions, discharges and transfers, and ones who are part of the care team, attending rounds with physicians and being available to patients at the push of the button. -
 Your career in Images Services at 91В鶹№ъІъѕ«Ж·ЧФЕД Explore a career in Imaging Services and learn how to grow your career in healthcare.
Your career in Images Services at 91В鶹№ъІъѕ«Ж·ЧФЕД Explore a career in Imaging Services and learn how to grow your career in healthcare. -
 Elevate your career as a Surgical Tech with 91В鶹№ъІъѕ«Ж·ЧФЕД As a surgical technician at 91В鶹№ъІъѕ«Ж·ЧФЕД, you will play a vital role in guaranteeing that surgical procedures are safe and successful. You will collaborate with leading surgeons and healthcare experts in cutting-edge facilities, providing our patients with the utmost care.
Elevate your career as a Surgical Tech with 91В鶹№ъІъѕ«Ж·ЧФЕД As a surgical technician at 91В鶹№ъІъѕ«Ж·ЧФЕД, you will play a vital role in guaranteeing that surgical procedures are safe and successful. You will collaborate with leading surgeons and healthcare experts in cutting-edge facilities, providing our patients with the utmost care. -
 Virtual Command Center Ever wondered what it was like to work in a Virtual Command Center? We’re in the background continuously assessing, reviewing and providing interventions to patients at all hours of the day across the nation.
Virtual Command Center Ever wondered what it was like to work in a Virtual Command Center? We’re in the background continuously assessing, reviewing and providing interventions to patients at all hours of the day across the nation.
Equal Opportunity
91В鶹№ъІъѕ«Ж·ЧФЕД™ is an Equal Opportunity/Affirmative Action employer committed to a diverse and inclusive workforce. All qualified applicants will be considered for employment without regard to race, color, religion, sex, sexual orientation, gender identity, national origin, age, disability, marital status, parental status, ancestry, veteran status, genetic information, or any other characteristic protected by law.
91В鶹№ъІъѕ«Ж·ЧФЕД™ will not discharge or in any other manner discriminate against employees or applicants because they have inquired about, discussed, or disclosed their pay or the pay of another employee or applicant. However, employees who have access to the compensation information of other employees or applicants as a part of their essential job functions cannot disclose the pay of other employees or applicants to individuals who do not otherwise have access to compensation information, unless the disclosure is (a) in response to a formal complaint or charge, (b) in furtherance of an investigation, proceeding, hearing, or action, including an investigation conducted by the employer, or (c) consistent with the contractor’s legal duty to furnish information. 41 CFR 60-1.35(c). External hires must pass a post-offer, pre-employment background check/drug screen. Qualified applicants with an arrest and/or conviction will be considered for employment in a manner consistent with federal and state laws, as well as applicable local ordinances, ban the box laws, including but not limited to the San Francisco and Los Angeles Fair Chance Ordinances. If you need a reasonable accommodation for any part of the employment process, please contact us by telephone at (415) 438-5575 and let us know the nature of your request. We will only respond to messages left that involve a request for a reasonable accommodation in the application process. We will accommodate the needs of any qualified candidate who requests a reasonable accommodation under the Americans with Disabilities Act (ADA). 91В鶹№ъІъѕ«Ж·ЧФЕД™ participates in E-Verify.